Services
- Treatment Overview
- Root Canal Therapy
- Endodontic Retreatment
- Endodontic Surgery
- Cracked Teeth
- Traumatic Injuries
- Advanced Technology
Treatment Overview
As an endodontic patient, what should I expect?
Dr. Elena will perform a comprehensive examination of your teeth to aid in diagnosing your pain and pulpal injury and determine if the tooth is a good candidate for endodontic therapy. She will provide a complete explanation of your diagnosis and treatment options as well as a review of any anticipated follow up with our office or your general dentist.
If needed, non-surgical root canal treatment will be performed under the microscope by Dr. Elena to eliminate the diseased pulp. This injured pulp is removed from within your tooth and the root canal system is thoroughly cleaned and sealed.
Under certain circumstances, endodontic retreatment or endodontic microsurgery may be indicated. Due to their complexity, oftentimes these will be performed at a separate appointment. We are experts in performing these procedures, and utilize sophisticated equipment to ensure the best results.
Endodontic Presentation
To provide you with a better understanding of endodontic procedures, we have provided the following multimedia presentation. Many common questions pertaining to root canal therapy are discussed.
Root Canal Therapy
What is a root canal?
At the center of your tooth is pulp. The pulp (or “nerve”) is a collection of blood vessels, connective tissue, and nerves that helped to build the surrounding tooth. Irritation to the pulp can be caused by trauma to the tooth, deep decay, cracks, or repeated dental procedures. Symptoms of the inflamed or infected pulp can be identified as sensitivity to temperature, chewing, spontaneous pain in the tooth and gums and swelling.
If you experience any of these symptoms, your dentist will most likely recommend non-surgical root canal treatment to eliminate the diseased pulp. The injured pulp tissue is removed and the root canal system is thoroughly cleaned and sealed. This therapy usually involves only local anesthesia (“novocaine”) and is usually completed in one visit depending on the treatment required. The success rate for this type of treatment is over 90%. If your tooth is not amenable to endodontic treatment or the chance of success is unfavorable, you will be informed by Dr. Elena at your consultation or if a complication becomes evident during or after treatment. In this event, there are other procedures that may be required. We use special deep numbing local anesthesia techniques to prevent discomfort during your treatment. We also provide other patient comfort items to help you relax during your procedure. You will be able to drive home after your treatment, and you probably will be comfortable returning to your normal routine.
Endodontic Presentation
To provide you with a better understanding of endodontic procedures, we have provided the following multimedia presentation. Many common questions pertaining to root canal therapy are discussed.
What happens after treatment?
When your root canal therapy has been completed, a record of your treatment will be sent to your restorative dentist. You should contact their office for a follow-up restoration within a few weeks of completion at our office. Your restorative dentist will decide on what type of restoration is necessary to protect your tooth. It is rare for endodontic patients to experience complications after routine endodontic treatment or microsurgery. If a problem does occur, however, we are available at all times to respond. To prevent further decay, continue to practice good dental hygiene.
Endodontic Retreatment
With the appropriate care, your teeth that have had endodontic treatment will last as long as other natural teeth. Yet, a tooth that has received treatment may fail to heal or pain may continue to exist. Sometimes, the pain may occur months or years after treatment. If so, Endodontic Retreatment may be needed.
With the appropriate care, your teeth that have had endodontic treatment will last as long as other natural teeth. Yet, a tooth that has received treatment may fail to heal or pain may continue to exist. Sometimes, the pain may occur months or years after treatment. If so, Endodontic Retreatment may be needed.
Improper healing may be caused by:
- Curved or narrow canals that were not treated during the initial treatment.
Complicated canals that went undetected during the initial treatment.
The crown or restoration was not placed within the appropriate amount of time following the procedure.
The crown or restoration that did not prevent saliva from contaminating the inside of the tooth.
In some cases, new problems can influence a tooth that was successfully treated:
- New decay can expose a root canal filling material, causing infection.
- A cracked or loose filling or crown can expose the tooth to new infection.
If retreatment is recommended, the doctor will reopen your tooth to gain access to the root canal filling material. This material will be removed to enable access to the root canal system. The doctor will now carefully examine the inside of the problematic tooth under the microscope and reclean the contaminated canal spaces. Once cleaned, the doctor will fill and seal the canals and place a filling in the biting surface of the tooth. If the tooth has already had a crown, the doctor may place a permanent restoration to seal your tooth. If no permanent crown is present or there is a problem discovered with your crown, you will need to return to your dentist to have a new crown placed to restore full functionality.
At this point, you will need to return to your dentist as soon as possible in order to have a new crown or restoration placed on the tooth to restore full functionality.
Endodontic Surgery
Why would I need Endodontic Surgery?
Generally, a root canal is all that is needed to save teeth with injured pulp from extraction. Occasionally, this non-surgical procedure will not be sufficient to heal the tooth and your endodontist will recommend surgery. Endodontic surgery can be used to locate fractures or hidden canals that do not appear on x-rays but still manifest pain in the tooth. Damaged root surfaces or the surrounding bone may also be treated with this procedure. The most common surgery used to save damaged teeth is an apicoectomy or root-end resection.
Generally, a root canal is all that is needed to save teeth with injured pulp from extraction. Occasionally, this non-surgical procedure will not be sufficient to heal the tooth and your endodontist will recommend surgery. Endodontic surgery can be used to locate fractures or hidden canals that do not appear on x-rays but still manifest pain in the tooth. Damaged root surfaces or the surrounding bone may also be treated with this procedure. The most common surgery used to save damaged teeth is an apicoectomy or root-end resection.
What is an Endodontic Surgery?
The video on the right illustrates this simple procedure. An incision is made in the gum tissue to expose the bone and inflamed soft tissue. The damaged tissue is removed along with the end of the root tip. A biocompatible root-end filling is placed to prevent reinfection of the root and the gum is sutured. The bone naturally heals around the root over a period of months restoring full function.
1.Infected Tissue
3. Suture Placed
2. Tissue Removed
4. Healing Complete
Following the procedure, there may be some discomfort or slight swelling while the incision heals. This is normal for any surgical procedure. To alleviate any discomfort, an appropriate pain medication will be recommended. If you have pain that does not respond to medication, please call our office.
Cracked Teeth
Cracked teeth demonstrate many types of symptoms, including pain when chewing, temperature sensitivities, or even the release of biting pressure. It is also common for pain to come and go, making it difficult to diagnose the cause of discomfort.
Cracked teeth demonstrate many types of symptoms, including pain when chewing, temperature sensitivities, or even the release of biting pressure. It is also common for pain to come and go, making it difficult to diagnose the cause of discomfort.
Chewing can cause movement of the cracked pieces of your tooth, and the pulp within the tooth becomes irritated. At the same time, when biting pressure is released, the crack can close quickly, resulting in sharp pain. Eventually, the pulp will become damaged and tooth will consistently hurt, even when you are not chewing. It is possible that cracks can lead to infection of the pulp tissue, which can spread to the bone and gum surrounding the problematic tooth.
Types of Cracks
Craze lines
These are tiny cracks that only affect the outer enamel of the tooth. These cracks are more common in adults. These types of cracks are superficial and are usually of no concern.
Fractured Cusp
When a cusp becomes weakened, a fracture may result. The cusp may break off or be removed by a dentist. A fractured cusp rarely damages the pulp, so root canal is not necessary. Your dentist will usually restore the tooth with a full crown.
Treatable Cracked Tooth
This type of crack extends from the chewing surface of the tooth and vertically migrates towards the root. In some cases, the crack may extend below the gum line. It is possible for the crack to extend further into the root. Damage to the pulp is commonplace. In this case, root canal treatment is usually necessary. A cracked tooth that is not treated will worsen, resulting in the loss of the tooth. Therefore, early detection is essential.
Split Tooth
A split tooth is usually the result of an untreated cracked tooth. It can be identified by a crack with distinct segments. This type of tooth can never be saved intact. Yet, the position and extent of the problem will dictate whether any portion of the tooth can be saved. Sometimes, endodontic retreatment by the doctors and restoration by your dentist can be used to save a portion of the tooth.
Verticle Root Fracture
A vertical root fracture begins at the root and extends towards the chewing surface of the tooth. Unfortunately, they show minimal symptoms and may go unnoticed. Treatment involves endodontic surgery if a portion of the tooth can be saved by removal of the fractured root. Otherwise the tooth will have to be extracted.
Traumatic Injuries
Dislodged Teeth
Injuries to the mouth can cause teeth to be pushed back into their sockets. Your endodontist or general dentist may reposition and stabilize your tooth. Root canal treatment is usually started within a few weeks of the injury and a medication, such as calcium hydroxide, will be placed inside the tooth. Eventually, a permanent root canal filling will be implanted.
Injuries to the mouth can cause teeth to be pushed back into their sockets. Your endodontist or general dentist may reposition and stabilize your tooth. Root canal treatment is usually started within a few weeks of the injury and a medication, such as calcium hydroxide, will be placed inside the tooth. Eventually, a permanent root canal filling will be implanted.
Sometimes a tooth may be pushed partially out of the socket. Again, your endodontist or general dentist may reposition and stabilize your tooth. If the pulp remains healthy, then no other treatment is necessary. Yet, if the pulp becomes damaged or infected, root canal treatment will be required. If left untreated, many different complications can arise. These complications can include but are not limited to: Infection of the tooth, root system or surrounding tissue, inadequate hygiene due to an inability to properly clean the dislodged tooth and the gums, and loss of the tooth.
Avulsed Teeth
If an injury causes a tooth to be completely knocked out of your mouth, it is important that you are treated immediately! If this happens to you, keep the tooth moist. If possible, put it back into the socket. A tooth can be saved if it remains moist. You can even put the tooth in milk or a glass of water (add a pinch of salt.) Your Endodontist may start root canal treatment based upon the stage of root development. The length of time the tooth was out of your mouth and the way the tooth was stored, may influence the type of treatment you receive.
If an injury causes a tooth to be completely knocked out of your mouth, it is important that you are treated immediately! If this happens to you, keep the tooth moist. If possible, put it back into the socket. A tooth can be saved if it remains moist. You can even put the tooth in milk or a glass of water (add a pinch of salt.) Your Endodontist may start root canal treatment based upon the stage of root development. The length of time the tooth was out of your mouth and the way the tooth was stored, may influence the type of treatment you receive.
Injuries in children
An injured immature tooth may need one of the following procedures to improve the chances of saving the tooth:
Apexogenesis
This procedure encourages the root to continue development as the pulp is healed. Soft tissue is covered with medication to encourage growth. The tip of the root (apex) will continue to close as the child gets older. In turn, the walls of the root canal will thicken. If the pulp heals, no additional treatment will be necessary. The more mature the root becomes, the better the chance to save the tooth.
Apexification
In this case, the unhealthy pulp is removed. The doctors place medication into the root to help a hard tissue form near the root tip. This hardened tissue provides a barrier for the root canal filling. At this point, the root canal walls will not continue to develop, making the tooth susceptible to fractures. So it is important to have the tooth properly restored by your dentist.
Pulp Regenerative Procedure
This is the latest in specialized endodontic treatments. In this case, the pulp tissue in the tooth has died prior to root end development, leaving a thin wide open root tip. The goal is to use the body’s own cells, which live beyond the tooth, to start regrowing pulp-like material in the tooth. A special cleaning protocol is used and special materials which allow these cells to regrow. If successful, this procedure allows for thickening of the root walls which provides for a stronger tooth in the future.
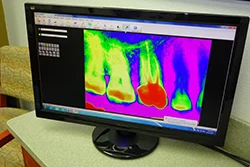
Advanced Technology
Patient Benefits
Our specialty practice is committed to excellence and using the latest state-of-the-art technology available to enhance patient care. Advanced training and use of new technologies result in a positive patient experience and make root canal treatment more effective and predictable. By using these advancements Dr. Elena is able to render a more conservative treatment while providing for a thorough, biologically sound treatment of your tooth.
The following are some of the important advances we use to better serve our patients:

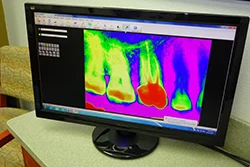
By using computerized digital x-rays, we can reduce the radiation to our patients by nearly 90%. A comfortable sensor pad is used, instead of film, to capture an instant image, which also means shorter appointments for our patients. Because they’re digital, these x-rays can be enhanced by the computer for improved visualization and diagnosis. A printed report, including these x-rays, is sent to your dentist after your visit with us.
Dr. Elena uses a special microscope during treatment to allow for enhanced vision through illumination and magnification. This technology greatly improves the doctor and assistant’s view inside the tooth facilitating a more thorough treatment, especially in locating calcified canals and diagnosing root fractures.
Through the microscope we are able to take digital pictures of your tooth. These pictures can be sent to your dentist for increased communication of your specific needs. This helps bridge the gap between our office and your referring dentist.
Instead of using a drill inside your tooth, this device vibrates a diamond coated metal tip at high frequency. Because it is very small, it can be used under the microscope for precise removal of small amounts of tooth or fillings, allowing for conservative treatment of your tooth. Dr. Elena also uses quiet electric handpieces (drills) to help eliminate the sound of the dental drill.
This device helps Dr. Elena to precisely measure the length of the tooth’s roots electronically for complete cleaning of the tooth. Since it is very accurate, it reduces the number of x-rays normally needed during the procedure. Used along with digital x-rays, this device lowers patient radiation exposure even further. The use of advanced training with new technologies help us to provide treatment that is safer, faster and more effective for our patients.
Cleaning of the root canal space and its many minute complexities is an important aspect to a successful outcome. Dr. Elena uses a device that utilizes sonic energy to energize irrigating solutions to help disrupt and remove pulp debris and bacteria from the root canal spaces.
Root canal cements or sealers from the past were irritating to the surrounding tissues. Dr. Elena uses a 100% biocompatible sealing material called Bioceramic, which assures the best seal while having been shown to be nontoxic, antimicrobial, causing minimal inflammation and also stimulating bone growth. This material provides your body an excellent chance to repair itself following our treatment and restore function to your tooth.
Having access to Cone Beam CT imaging allows Dr. Elena the capabilities to see your tooth in 3D. This aids her in detecting and treating complex root anatomy, calcified and extra canals in your tooth that would not be easily seen by conventional 2D digital x-rays. It can also help in complex diagnosis of more difficult cases such as upper teeth near the sinus cavity and cheek bone where traditional x-rays can sometimes be limited. Watch video here.
Conserving tooth structure during the root canal procedures is important to avoid weakening of the root and potential tooth fractures. Recent scientific improvements in material science has provided us a revolutionary advancement in root canal therapy through an instrument called TruShape 3D Conforming Files (Dentsply Inc.). Due to their decreasing taper and unique shape, these instruments remove less of the tooth during use as compared to standard file instruments. Since it contacts a higher percentage of the canal wall, more bacteria are removed by the disruption of their home or “biofilm”. The super elastic properties of this instrument can adapt to different canal shapes by flattening in small, narrow parts of the canal while expanding into wider more ribbon shaped areas. TruShape files are designed for use by endodontic specialists and training is required prior to utilizing the instruments in a clinical setting. We are excited to offer our patients the benefits of treatment with this cutting edge technology as it offers a truly unique advancement in root canal therapy.
Lasers allow for highly precise targeting of affected areas, minimizing damage to surrounding healthy tissues. This precision leads to more effective treatments and faster recovery times. Laser-assisted irrigation significantly improves the cleaning and disinfection of root canals. It eradicates bacteria more effectively than traditional methods, reducing the risk of reinfection. Using lasers can shorten the duration of endodontic procedures. The efficiency of laser technology means less time in the chair for patients, enhancing their overall experience. Lasers offer a minimally invasive approach to endodontic treatments. They selectively target diseased tissue while preserving as much healthy tissue as possible, leading to less postoperative discomfort and quicker healing. Patients often experience less pain and discomfort during and after laser treatments compared to conventional methods. This can lead to higher patient satisfaction and better overall outcomes. The use of lasers reduces the need for mechanical instruments, lowering the risk of procedural errors and improving the safety of endodontic treatments.
- Treatment Overview
- Root Canal Therapy
- Endodontic Retreatment
- Endodontic Surgery
- Cracked Teeth
- Traumatic Injuries
- Advanced Technology
Treatment Overview
As an endodontic patient, what should I expect?
Dr. Elena will perform a comprehensive examination of your teeth to aid in diagnosing your pain and pulpal injury and determine if the tooth is a good candidate for endodontic therapy. She will provide a complete explanation of your diagnosis and treatment options as well as a review of any anticipated follow up with our office or your general dentist.
If needed, non-surgical root canal treatment will be performed under the microscope by Dr. Elena to eliminate the diseased pulp. This injured pulp is removed from within your tooth and the root canal system is thoroughly cleaned and sealed.
Under certain circumstances, endodontic retreatment or endodontic microsurgery may be indicated. Due to their complexity, oftentimes these will be performed at a separate appointment. We are experts in performing these procedures, and utilize sophisticated equipment to ensure the best results.
Endodontic Presentation
To provide you with a better understanding of endodontic procedures, we have provided the following multimedia presentation. Many common questions pertaining to root canal therapy are discussed.
Root Canal Therapy
What is a root canal?
At the center of your tooth is pulp. The pulp (or “nerve”) is a collection of blood vessels, connective tissue, and nerves that helped to build the surrounding tooth. Irritation to the pulp can be caused by trauma to the tooth, deep decay, cracks, or repeated dental procedures. Symptoms of the inflamed or infected pulp can be identified as sensitivity to temperature, chewing, spontaneous pain in the tooth and gums and swelling.
If you experience any of these symptoms, your dentist will most likely recommend non-surgical root canal treatment to eliminate the diseased pulp. The injured pulp tissue is removed and the root canal system is thoroughly cleaned and sealed. This therapy usually involves only local anesthesia (“novocaine”) and is usually completed in one visit depending on the treatment required. The success rate for this type of treatment is over 90%. If your tooth is not amenable to endodontic treatment or the chance of success is unfavorable, you will be informed by Dr. Elena at your consultation or if a complication becomes evident during or after treatment. In this event, there are other procedures that may be required. We use special deep numbing local anesthesia techniques to prevent discomfort during your treatment. We also provide other patient comfort items to help you relax during your procedure. You will be able to drive home after your treatment, and you probably will be comfortable returning to your normal routine.
Endodontic Presentation
To provide you with a better understanding of endodontic procedures, we have provided the following multimedia presentation. Many common questions pertaining to root canal therapy are discussed.
What happens after treatment?
When your root canal therapy has been completed, a record of your treatment will be sent to your restorative dentist. You should contact their office for a follow-up restoration within a few weeks of completion at our office. Your restorative dentist will decide on what type of restoration is necessary to protect your tooth. It is rare for endodontic patients to experience complications after routine endodontic treatment or microsurgery. If a problem does occur, however, we are available at all times to respond. To prevent further decay, continue to practice good dental hygiene.
Endodontic Retreatment
With the appropriate care, your teeth that have had endodontic treatment will last as long as other natural teeth. Yet, a tooth that has received treatment may fail to heal or pain may continue to exist. Sometimes, the pain may occur months or years after treatment. If so, Endodontic Retreatment may be needed.
With the appropriate care, your teeth that have had endodontic treatment will last as long as other natural teeth. Yet, a tooth that has received treatment may fail to heal or pain may continue to exist. Sometimes, the pain may occur months or years after treatment. If so, Endodontic Retreatment may be needed.
Improper healing may be caused by:
- Curved or narrow canals that were not treated during the initial treatment.
Complicated canals that went undetected during the initial treatment.
The crown or restoration was not placed within the appropriate amount of time following the procedure.
The crown or restoration that did not prevent saliva from contaminating the inside of the tooth.
In some cases, new problems can influence a tooth that was successfully treated:
- New decay can expose a root canal filling material, causing infection.
- A cracked or loose filling or crown can expose the tooth to new infection.
If retreatment is recommended, the doctor will reopen your tooth to gain access to the root canal filling material. This material will be removed to enable access to the root canal system. The doctor will now carefully examine the inside of the problematic tooth under the microscope and reclean the contaminated canal spaces. Once cleaned, the doctor will fill and seal the canals and place a filling in the biting surface of the tooth. If the tooth has already had a crown, the doctor may place a permanent restoration to seal your tooth. If no permanent crown is present or there is a problem discovered with your crown, you will need to return to your dentist to have a new crown placed to restore full functionality.
At this point, you will need to return to your dentist as soon as possible in order to have a new crown or restoration placed on the tooth to restore full functionality.
Endodontic Surgery
Why would I need Endodontic Surgery?
Generally, a root canal is all that is needed to save teeth with injured pulp from extraction. Occasionally, this non-surgical procedure will not be sufficient to heal the tooth and your endodontist will recommend surgery. Endodontic surgery can be used to locate fractures or hidden canals that do not appear on x-rays but still manifest pain in the tooth. Damaged root surfaces or the surrounding bone may also be treated with this procedure. The most common surgery used to save damaged teeth is an apicoectomy or root-end resection.
Generally, a root canal is all that is needed to save teeth with injured pulp from extraction. Occasionally, this non-surgical procedure will not be sufficient to heal the tooth and your endodontist will recommend surgery. Endodontic surgery can be used to locate fractures or hidden canals that do not appear on x-rays but still manifest pain in the tooth. Damaged root surfaces or the surrounding bone may also be treated with this procedure. The most common surgery used to save damaged teeth is an apicoectomy or root-end resection.
What is an Endodontic Surgery?
The video on the right illustrates this simple procedure. An incision is made in the gum tissue to expose the bone and inflamed soft tissue. The damaged tissue is removed along with the end of the root tip. A biocompatible root-end filling is placed to prevent reinfection of the root and the gum is sutured. The bone naturally heals around the root over a period of months restoring full function.
1.Infected Tissue
3. Suture Placed
2. Tissue Removed
4. Healing Complete
Following the procedure, there may be some discomfort or slight swelling while the incision heals. This is normal for any surgical procedure. To alleviate any discomfort, an appropriate pain medication will be recommended. If you have pain that does not respond to medication, please call our office.
Cracked Teeth
Cracked teeth demonstrate many types of symptoms, including pain when chewing, temperature sensitivities, or even the release of biting pressure. It is also common for pain to come and go, making it difficult to diagnose the cause of discomfort.
Cracked teeth demonstrate many types of symptoms, including pain when chewing, temperature sensitivities, or even the release of biting pressure. It is also common for pain to come and go, making it difficult to diagnose the cause of discomfort.
Chewing can cause movement of the cracked pieces of your tooth, and the pulp within the tooth becomes irritated. At the same time, when biting pressure is released, the crack can close quickly, resulting in sharp pain. Eventually, the pulp will become damaged and tooth will consistently hurt, even when you are not chewing. It is possible that cracks can lead to infection of the pulp tissue, which can spread to the bone and gum surrounding the problematic tooth.
Types of Cracks
Craze lines
These are tiny cracks that only affect the outer enamel of the tooth. These cracks are more common in adults. These types of cracks are superficial and are usually of no concern.
Fractured Cusp
When a cusp becomes weakened, a fracture may result. The cusp may break off or be removed by a dentist. A fractured cusp rarely damages the pulp, so root canal is not necessary. Your dentist will usually restore the tooth with a full crown.
Treatable Cracked Tooth
This type of crack extends from the chewing surface of the tooth and vertically migrates towards the root. In some cases, the crack may extend below the gum line. It is possible for the crack to extend further into the root. Damage to the pulp is commonplace. In this case, root canal treatment is usually necessary. A cracked tooth that is not treated will worsen, resulting in the loss of the tooth. Therefore, early detection is essential.
Split Tooth
A split tooth is usually the result of an untreated cracked tooth. It can be identified by a crack with distinct segments. This type of tooth can never be saved intact. Yet, the position and extent of the problem will dictate whether any portion of the tooth can be saved. Sometimes, endodontic retreatment by the doctors and restoration by your dentist can be used to save a portion of the tooth.
Verticle Root Fracture
A vertical root fracture begins at the root and extends towards the chewing surface of the tooth. Unfortunately, they show minimal symptoms and may go unnoticed. Treatment involves endodontic surgery if a portion of the tooth can be saved by removal of the fractured root. Otherwise the tooth will have to be extracted.
Traumatic Injuries
Dislodged Teeth
Injuries to the mouth can cause teeth to be pushed back into their sockets. Your endodontist or general dentist may reposition and stabilize your tooth. Root canal treatment is usually started within a few weeks of the injury and a medication, such as calcium hydroxide, will be placed inside the tooth. Eventually, a permanent root canal filling will be implanted.
Injuries to the mouth can cause teeth to be pushed back into their sockets. Your endodontist or general dentist may reposition and stabilize your tooth. Root canal treatment is usually started within a few weeks of the injury and a medication, such as calcium hydroxide, will be placed inside the tooth. Eventually, a permanent root canal filling will be implanted.
Sometimes a tooth may be pushed partially out of the socket. Again, your endodontist or general dentist may reposition and stabilize your tooth. If the pulp remains healthy, then no other treatment is necessary. Yet, if the pulp becomes damaged or infected, root canal treatment will be required. If left untreated, many different complications can arise. These complications can include but are not limited to: Infection of the tooth, root system or surrounding tissue, inadequate hygiene due to an inability to properly clean the dislodged tooth and the gums, and loss of the tooth.
Avulsed Teeth
If an injury causes a tooth to be completely knocked out of your mouth, it is important that you are treated immediately! If this happens to you, keep the tooth moist. If possible, put it back into the socket. A tooth can be saved if it remains moist. You can even put the tooth in milk or a glass of water (add a pinch of salt.) Your Endodontist may start root canal treatment based upon the stage of root development. The length of time the tooth was out of your mouth and the way the tooth was stored, may influence the type of treatment you receive.
If an injury causes a tooth to be completely knocked out of your mouth, it is important that you are treated immediately! If this happens to you, keep the tooth moist. If possible, put it back into the socket. A tooth can be saved if it remains moist. You can even put the tooth in milk or a glass of water (add a pinch of salt.) Your Endodontist may start root canal treatment based upon the stage of root development. The length of time the tooth was out of your mouth and the way the tooth was stored, may influence the type of treatment you receive.
Injuries in children
An injured immature tooth may need one of the following procedures to improve the chances of saving the tooth:
Apexogenesis
This procedure encourages the root to continue development as the pulp is healed. Soft tissue is covered with medication to encourage growth. The tip of the root (apex) will continue to close as the child gets older. In turn, the walls of the root canal will thicken. If the pulp heals, no additional treatment will be necessary. The more mature the root becomes, the better the chance to save the tooth.
Apexification
In this case, the unhealthy pulp is removed. The doctors place medication into the root to help a hard tissue form near the root tip. This hardened tissue provides a barrier for the root canal filling. At this point, the root canal walls will not continue to develop, making the tooth susceptible to fractures. So it is important to have the tooth properly restored by your dentist.
Pulp Regenerative Procedure
This is the latest in specialized endodontic treatments. In this case, the pulp tissue in the tooth has died prior to root end development, leaving a thin wide open root tip. The goal is to use the body’s own cells, which live beyond the tooth, to start regrowing pulp-like material in the tooth. A special cleaning protocol is used and special materials which allow these cells to regrow. If successful, this procedure allows for thickening of the root walls which provides for a stronger tooth in the future.
Advanced Technology
Patient Benefits
Our specialty practice is committed to excellence and using the latest state-of-the-art technology available to enhance patient care. Advanced training and use of new technologies result in a positive patient experience and make root canal treatment more effective and predictable. By using these advancements Dr. Elena is able to render a more conservative treatment while providing for a thorough, biologically sound treatment of your tooth.
The following are some of the important advances we use to better serve our patients:

By using computerized digital x-rays, we can reduce the radiation to our patients by nearly 90%. A comfortable sensor pad is used, instead of film, to capture an instant image, which also means shorter appointments for our patients. Because they’re digital, these x-rays can be enhanced by the computer for improved visualization and diagnosis. A printed report, including these x-rays, is sent to your dentist after your visit with us.
Dr. Elena uses a special microscope during treatment to allow for enhanced vision through illumination and magnification. This technology greatly improves the doctor and assistant’s view inside the tooth facilitating a more thorough treatment, especially in locating calcified canals and diagnosing root fractures.
Through the microscope we are able to take digital pictures of your tooth. These pictures can be sent to your dentist for increased communication of your specific needs. This helps bridge the gap between our office and your referring dentist.
Instead of using a drill inside your tooth, this device vibrates a diamond coated metal tip at high frequency. Because it is very small, it can be used under the microscope for precise removal of small amounts of tooth or fillings, allowing for conservative treatment of your tooth. Dr. Elena also uses quiet electric handpieces (drills) to help eliminate the sound of the dental drill.
This device helps Dr. Elena to precisely measure the length of the tooth’s roots electronically for complete cleaning of the tooth. Since it is very accurate, it reduces the number of x-rays normally needed during the procedure. Used along with digital x-rays, this device lowers patient radiation exposure even further. The use of advanced training with new technologies help us to provide treatment that is safer, faster and more effective for our patients.
Cleaning of the root canal space and its many minute complexities is an important aspect to a successful outcome. Dr. Elena uses a device that utilizes sonic energy to energize irrigating solutions to help disrupt and remove pulp debris and bacteria from the root canal spaces.
Root canal cements or sealers from the past were irritating to the surrounding tissues. Dr. Elena uses a 100% biocompatible sealing material called Bioceramic, which assures the best seal while having been shown to be nontoxic, antimicrobial, causing minimal inflammation and also stimulating bone growth. This material provides your body an excellent chance to repair itself following our treatment and restore function to your tooth.
Having access to Cone Beam CT imaging allows Dr. Elena the capabilities to see your tooth in 3D. This aids her in detecting and treating complex root anatomy, calcified and extra canals in your tooth that would not be easily seen by conventional 2D digital x-rays. It can also help in complex diagnosis of more difficult cases such as upper teeth near the sinus cavity and cheek bone where traditional x-rays can sometimes be limited. Watch video here.
Conserving tooth structure during the root canal procedures is important to avoid weakening of the root and potential tooth fractures. Recent scientific improvements in material science has provided us a revolutionary advancement in root canal therapy through an instrument called TruShape 3D Conforming Files (Dentsply Inc.). Due to their decreasing taper and unique shape, these instruments remove less of the tooth during use as compared to standard file instruments. Since it contacts a higher percentage of the canal wall, more bacteria are removed by the disruption of their home or “biofilm”. The super elastic properties of this instrument can adapt to different canal shapes by flattening in small, narrow parts of the canal while expanding into wider more ribbon shaped areas. TruShape files are designed for use by endodontic specialists and training is required prior to utilizing the instruments in a clinical setting. We are excited to offer our patients the benefits of treatment with this cutting edge technology as it offers a truly unique advancement in root canal therapy.
Lasers allow for highly precise targeting of affected areas, minimizing damage to surrounding healthy tissues. This precision leads to more effective treatments and faster recovery times. Laser-assisted irrigation significantly improves the cleaning and disinfection of root canals. It eradicates bacteria more effectively than traditional methods, reducing the risk of reinfection. Using lasers can shorten the duration of endodontic procedures. The efficiency of laser technology means less time in the chair for patients, enhancing their overall experience. Lasers offer a minimally invasive approach to endodontic treatments. They selectively target diseased tissue while preserving as much healthy tissue as possible, leading to less postoperative discomfort and quicker healing. Patients often experience less pain and discomfort during and after laser treatments compared to conventional methods. This can lead to higher patient satisfaction and better overall outcomes. The use of lasers reduces the need for mechanical instruments, lowering the risk of procedural errors and improving the safety of endodontic treatments.